妊娠糖尿病(gestational diabetes mellitus,GDM)是一种妇女在妊娠期间由于糖代谢紊乱等原因而导致首次出现的糖尿病。妊娠中后期机体出现轻微的胰岛素抵抗(insulin resistance,IR),使体内血糖水平升高,以保证给胎儿供给充足的葡萄糖,而异常增多的IR则会对孕妇生理代谢与胎儿生长发育造成严重危害,因此将孕期严重的葡萄糖耐量受损定义为妊娠糖尿病。妊娠糖尿病导致的孕妇短期妊娠风险(如死产、早产、巨大儿、新生儿低血糖、新生儿高胆红素血症等)与长期风险(如亲代与子代的肥胖、胰岛素抵抗、糖耐量异常等)均比健康孕妇更高。中国的妊娠糖尿病总发病率约为14.8%,可能是患者数量最多的国家[1]。鉴于妊娠糖尿病的流行形势,了解其发病机制以及开发干预策略具有充分的必要性与重大意义。
妊娠糖尿病最主要的机制是IR,观察到患者的磷脂酰肌醇3-激酶(phosphatidylinositide 3-kinase,PI3K)途径中,胰岛素受体底物-1(insulin receptor substrate 1,IRS-1)、葡萄糖转运蛋白4(glucose transporter 4,GLUT4)、PI3K与蛋白激酶B(protein kinase B,PKB)等多种胰岛素信号传导介质表达受损[2]。妊娠期间机体发生的多种变化,如Toll样受体4(toll like receptor 4,TLR4)、p38丝裂原活化蛋白激酶(mitogen activated protein kinase,MAPK)的上调、PPARγ的下调,以及肠道菌群的结构紊乱等,共同促进NF-κB、TNF-α、IL-1、IL-6等炎症因子的释放,是IR与妊娠糖尿病的重要促进因素[3-6]。这些炎症因子诱导IR的机制包括通过抑制胰岛素受体酪氨酸激酶的活性从而减少IRS-1的酪氨酸磷酸化,与通过诱导活性氧的生成来激活c-Jun氨基末端激酶(c-Jun N-teminal Kinase,JNK)通路从而增强IRS-1的丝氨酸磷酸化[4,7]。
了解妊娠糖尿病的发病机制对开发干预措施具有重要的指导意义,而膳食营养干预是治疗的重要组成部分。妊娠糖尿病的营养干预以限制热量的低升糖指数饮食为主,碳水化合物、脂质、蛋白质等供能营养素的摄入与供能比需要严格控制。而众多研究表明,在膳食营养干预基础上增加其他膳食成分,如膳食纤维、维生素、矿物质、不饱和脂肪酸、植物化学物等的摄入对妊娠糖尿病的改善效果更为显著。本文旨在综述这些膳食成分作为辅助干预措施对妊娠糖尿病的改善效果及其功能原理,以期为开发妊娠糖尿病的膳食干预策略提供参考依据。
1 碳水化合物
1.1 菊粉
菊粉是由β-D-呋喃果糖经β-1,2-糖苷键连接而成的线性直链多糖,其特殊的β-1,2-糖苷键使得菊粉不能在肠道中被消化,但能被肠道微生物利用。妊娠糖尿病孕妇连续4周每日服用10 g菊粉型果聚糖能显著降低HbA1c(-0.28% vs.-0.1%,P<0.01)、TG(+0.10 vs.+0.50 mmol/L,P<0.05)、TC(+0.40 vs.+0.60 mmol/L,P<0.05)与LDL-C(+0.14 vs.+0.58 mmol/L,P<0.05)[8]。服用菊粉抑制JNK通路并增强IRS与PKB的磷酸化,增强胰岛素敏感性,促进骨骼肌细胞与肝细胞摄取葡萄糖[9-10]。菊粉可提高肠道菌群丰度,改善肠道菌群结构,且其发酵产物短链脂肪酸(short chain fatty acids,SCFA)具有抗糖尿病活性,包括提高GLUT4转位与表达,促进AMPK和ACC的磷酸化,抑制JNK和NF-κB的激活以及SOCS3的表达[11-12]。
1.2 低聚果糖
低聚果糖是蔗糖分子以β-1,2-糖苷键与1~3个果糖分子结合构成的直链杂低聚糖,广泛存在于多种植物中。相比胰岛素治疗,每日服用20 g低聚果糖并联合个体化营养干预能更显著下调空腹血糖(fasting blood glucose,FBG)(-6.11 vs.-3.11 mmol/L,P<0.05)、2hPG(-7.92 vs.-3.48 mmol/L,P<0.05)与HbA1c(-3.49 vs.-2.00 mmol/L,P<0.05)[13]。此外,低聚果糖与二甲双胍常被联合用于临床治疗,部分患者可能需要联合用药强化治疗效果,且低聚果糖具有良好的安全性,能有效地辅助降糖药物发挥作用。与菊粉类似,低聚果糖只能被肠道微生物分解代谢为SCFAs,并选择性促进有益菌的生长,抑制有害菌,改善肠道菌群结构。
1.3 β-葡聚糖
β-葡聚糖是葡萄糖分子以β-1,3-糖苷键为主链,β-1,4-糖苷键或β-1,6-糖苷键为支链连接而成的一类碳水化合物,存在于燕麦、大麦等谷物以及酵母和真菌的细胞壁中。连续8周每日服用含4 g β-葡聚糖的燕麦能提高妊娠糖尿病孕妇肠道菌群Alpha多样性,降低FBG(-0.60 vs.-0.37 mmol/L,P<0.05)与身体质量指数(body mass index,BMI)增长(+4.56 vs.+5.34 kg/m2,P<0.05),但对妊娠结局无明显影响[14]。持续4周每天摄入30 g燕麦麸皮,同样改善妊娠糖尿病患者的FBG[(84.59±2.84) vs.(92.77±4.97) mg/dL,P<0.001]与2hPG[(104.04±5.48) vs.(117.49±11.34) mg/dL,P<0.001][15]。β-葡聚糖的网络状天然结构将蛋白质与淀粉包裹住,使其减少与消化酶的物理接触,从而抑制淀粉在肠道中的消化[16]。另外,β-葡聚糖促进小肠糖异生,提高胰岛素敏感性,抑制促进食欲的神经肽Y的分泌并提高抑制食欲的神经肽垂体前体阿黑皮素的分泌[17]。
1.4 小麦纤维素
人类膳食中的纤维素主要来自于蔬菜和粗加工的谷物,小麦中纤维素在一众谷物中含量较高,这可能是小麦纤维素在缓解妊娠糖尿病方面应用得较多的原因。妊娠糖尿病孕妇每日额外摄入7 g小麦纤维素,4周或8周后糖脂代谢状态得到显著的改善,且8周疗程在改善2hPG[(4.96±1.32) vs.(5.43±1.49)mmol/L]、TG[(2.08±0.85)vs.(3.62±0.74) mmol/L]与HOMA-IR[(1.06±0.75)vs.(1.84±1.06)mmol/L]方面优于4周疗程[18-19]。另有研究表明,持续2周每日额外摄入15 g小麦麸皮可减少胰岛素需求(38.9 %vs.76.9%,P=0.04)[20]。
2 维生素
2.1 维生素D
维生素D是一种脂溶性维生素,人类膳食摄入主要来源包括鱼肝油、蘑菇、奶酪与鸡蛋等。妊娠糖尿病孕妇每2周口服50 000 IU维生素D3,持续8周能够改善FBG(-4.72 vs.+5.27 mg/dL,P=0.01)与HbA1c(-0.18% vs.+0.17%,P=0.02),但对血脂与氧化应激水平没有显著影响[21]。另有研究发现,6周内2次服用50 000 IU维生素D3可显著降低羊水过多(0% vs.17.4%,P=0.04)与新生儿高胆红素血症(27.3% vs.60.9%,P=0.02)的风险[22]。维生素D诱导胰腺b细胞内Ca2+去极化增强胰岛素分泌,并通过抑制维生素D受体介导的NF-κB和MAPK信号通路来下调炎症因子的表达与上调PI3K和Akt的表达,以改善胰岛素敏感性[23-25]。维生素D还可降低NADPH的表达,增强SOD的表达,缓解氧化应激[23]。还观察到,维生素D可能通过肾素-血管紧张素-醛固酮系统间接缓解IR[23]。
2.2 B族维生素
B族维生素包括B1、B3、B6、B12、B9(叶酸)、Bh(肌醇)等,它们由于共同的特性(水溶性辅酶)与协同作用而被归类为一族。维生素B12与叶酸联合使用显著降低妊娠糖尿病患者的FBG[(4.0±0.5)vs.(4.8±0.7)mmol/L,P<0.01]、2hPG[(5.9±0.6)vs.(8.2±0.8)mmol/L,P<0.01]与HbA1c[(5.1±0.6)%vs.(6.5±0.8)%,P<0.01],并改善妊娠结局[26]。叶酸、维生素B6与甲钴胺联合治疗显著降低了患者FBG[(6.32±1.22)vs.(7.52±1.04) mmol/L,P=0.000)与2hPG[(8.64±2.33)vs.(10.01±2.17) mmol/L,P=0.005],并减少新生儿并发症(4.55%vs.20.45%,P=0.024)[27]。此外,每日服用2 g肌醇有助于达到控糖目标(89.8%vs.68%,P=0.008)[28],而每日服用4 g肌醇持续8周显著降低FBG[(4.6±0.3)vs.(5.1±0.3)mmol/L,P<0.05]、空腹胰岛素[(19.0±5.8) vs.(26.0±6.8) μIU/mL,P<0.05]与HOMA-IR[(3.5±1.1)vs.(5.3±1.4),P<0.05][29]。维生素B6通过抑制色氨酸分解代谢为犬尿氨酸,促进脂肪与AGE的合成来发挥抗糖尿病作用[30]。维生素B12可以增强糖尿病与肥胖的最强候选基因(TCF7L2和FTO)的甲基化,以减少该基因在糖尿病中的促进作用[31]。肌醇通过增强PPARγ的表达从而增强GLUT4和胰岛素受体的表达,以修复受损的PI3K途径[32]。此外,还观察到肌醇可以抑制肠道中葡萄糖的吸收,延迟胃排空,这可能与它有类似葡萄糖的结构而产生竞争性抑制相关[33]。
2.3 维生素E
维生素E是生育酚类物质的总称,是优良的抗氧化剂。妊娠糖尿病孕妇连续6天每日服用30 mg维生素E能有效降低FBG[(4.98±0.41)vs.(5.21±0.66)mmol/L,P=0.01]、2hPG[(7.99±0.27)vs.(8.34±0.23)mmol/L,P=0.01)与TG[(1.54±0.41)vs.(1.81±0.62)mmol/L,P=0.01],降低不良妊娠结局的风险[34]。而持续4周的维生素E摄入可以下调妊娠糖尿病孕妇的炎症因子CRP[(3.51±1.62)vs.(5.44±2.40)mg/L,P<0.05)、IL-6[(12.61±3.70) vs.(15.43±3.82)ng/L,P<0.05]与脂类TC[(3.17±0.49) vs.(4.17±0.52)mmol/L,P<0.05]、TG[(1.34±0.30)vs.(1.85±0.43)mol/L,P<0.05)[35]。维生素E修复因氧化应激受损的PPARγ的表达,进而增强脂联素的表达,从而提高胰岛素敏感性[36]。
2.4 α-硫辛酸
α-硫辛酸为双硫五元环维生素,普遍存在于动物肝脏、肾脏组织、菠菜与花椰菜等食物中。其抗氧化机制包括直接清除自由基、螯合金属阳离子、亲电子作用、诱导血红素加氧酶-1表达和增强生物体内其他抗氧化剂等[37]。此外,α-硫辛酸可以增强胰岛细胞中AMPK的活性与脂肪细胞中IRS-1和Akt磷酸化,改善胰岛素敏感性[38-39]。妊娠糖尿病孕妇每日摄入100 mg或300 mg α-硫辛酸,8周后显著下调FBG[(83.56±1.31)vs.(94.63±1.18)mg/dL,P<0.001]与TG[(221.15±6.91)vs.(248.33±11.01)mg/dL,P=0.041],并改善氧化应激状态[40]。
3 矿物质
3.1 锌
锌的膳食摄入来源主要是海产品、红色肉类与动物内脏等。每日口服25 mg硫酸锌,持续8周可改善GDM患者的血糖控制,减少对胰岛素的需求[(8.76±9.63) vs.(17.53±10.54) IU,P=0.001],以及减少巨大儿的发生率(6.7%vs.33.3%,P=0.01)[41]。而每日摄入30 mg锌,持续6周能够降低妊娠糖尿病孕妇FBG[(-6.6±11.2) vs.(+0.6±6.7) mg/dL,P=0.005]、血浆胰岛素[(-1.3±6.6)vs.(+6.6±12.2) μIU/mL,P=0.003]与HOMA-IR[(-0.5±1.6) vs.(+1.5±2.7),P=0.001][42]。锌发挥胰岛素样作用介导IRS-1酪氨酸磷酸化,抑制糖原合酶激酶-3β活性,增强糖原合酶活性,提高细胞对葡萄糖的摄取[43-44]。锌能直接与肠道中的α-葡萄糖苷酶结合,使其三级构象变化并失活,从而减少碳水化合物的吸收[45]。此外,锌是超氧化物歧化酶等关键抗氧化酶的辅助因子,有助于减少活性氧的合成,从而抑制氧化应激途径[46]。
3.2 硒
硒主要存在于动物内脏与海产品中。妊娠糖尿病孕妇每日补充200 mg硒补充剂,持续6周后FBG[(-10.5±11.9)vs.+ (4.5±12.9)mg/dL,P<0.001]、血浆胰岛素[(-1.98±11.25)vs.(5.26±9.33)μIU/mL,P=0.005]与HOMA-IR[(-0.84±2.76)vs.+(1.47±2.46),P<0.001]得到显著改善[47]。每日服用200 mg硒补充剂,持续6周能下调妊娠糖尿病孕妇炎症因子TNF-α(P=0.02)与TGF-β(P=0.01)的表达,上调PPARγ(P=0.03)和GLUT1(P=0.01)的表达,并减少新生儿高胆红素血症(5.6%vs.33.3%,P=0.03)与住院率(5.6%vs.33.3%,P=0.03)[48-49]。而每日服用100 mg硒补充剂,持续12周对妊娠糖尿病没有缓解作用[50]。硒通过组成硒依赖性谷胱甘肽过氧化物酶和其他硒蛋白参与构成氧化应激防御系统[51]。硒还能特异性上调胰岛素启动子1的基因表达,刺激胰岛细胞中胰岛素的分泌[52]。
3.3 镁
绿叶蔬菜中的叶绿素是镁的丰富来源,此外,镁也存在于粗粮、坚果、大豆和海产品中。妊娠糖尿病孕妇每日补充250 mg镁补充剂,持续6周后PPARγ(P=0.003)与GLUT1(P=0.004)的表达升高、FBG[(-9.7±5.6)vs.(-0.1±8.5)mg/dL,P<0.001]、炎症因子TNF-α(P=0.006)与IL-8(P=0.03)显著降低[53]。镁是胰岛素受体酪氨酸激酶、糖酵解酶与糖异生酶的辅因子,参与胰岛素信号传导与糖代谢[54]。镁还可减少脂肪组织中IL-1与TNF-α的分泌,缓解炎症[54]。镁通过增加ATP、降低线粒体活性氧和Ca2+超载,使线粒体膜电位复极来改善线粒体功能,缓解氧化应激[55]。
4 其他
4.1 Omega-3脂肪酸
Omega-3脂肪酸(ω-3 PUFAs)常存在于鱼类油脂和植物油中,是一组多不饱和脂肪酸,包括α-亚麻酸、二十碳五烯酸(eicosapentaenoic acid,EPA)和二十二碳六烯酸(docosahexaenoic acid,DHA)。ω-3 PUFAs有利于调节母婴代谢功能,而妊娠糖尿病患者的胎盘功能异常会影响ω-3 PUFAs的运输,从而影响胎儿生长发育[56]。此外,ω-3 PUFAs激活游离脂肪酸受体4使其磷酸化并与β-arrestin-2相互作用,使得β-arrestin-2与炎症通路的重要因子TAB1结合并中断炎症通路[57]。ω-3 PUFAs是促分解介质(如溶解素、保护素等)的前体,可减轻脂肪炎症并增强胰岛素敏感性[58]。ω-3 PUFAs可增强胰岛素转录因子表达,促进胰岛素分泌[59]。胎球蛋白A通过抑制胰岛素受体的酪氨酸激酶活性诱导IR,而摄入ω-3 PUFAs可降低血清胎球蛋白A水平[60]。妊娠糖尿病妇女连续6周每日服用含180 mg EPA与120 mg DHA的胶囊能显著下调FBG[(-4.4±2.3) vs.(+2.9±14.3) mg/dL,P=0.02]、血清胰岛素[(-1.5±7.5)vs.(+3.5±8.5) μIU/mL,P=0.02]、HOMA-IR(-0.4±2.1 vs.+1.1±2.4,P=0.02)[61]。此外,一项持续6周的研究显示,每日800 mg α-亚麻酸的摄入同样改善妊娠糖尿病孕妇的FBG[(84.6±6.8) vs.(90.6±5.0) mg/dL,P=0.001]、血浆胰岛素[(10.0±3.2)vs.(13.2±3.9) μIU/mL,P=0.001]与HOMA-IR(2.4±0.7 vs.3.0±1.0,P<0.001)[62]。
4.2 益生菌
益生菌是活的微生物,当摄入足够的量时,会给宿主带来健康益处。将嗜酸乳杆菌、干酪乳杆菌与两歧双歧杆菌(各2×109 CFU/g每日)联合治疗妊娠糖尿病,持续6周能够显著降低FBG[(-5.3±6.7)vs.(+0.03±9.0) mg/dL,P=0.01]、hs-CRP[((-2.2±2.7)vs.(+0.5±2.4) mg/mL,P<0.001)与MDA[(-0.1±0.8)vs.(+0.5±1.5)mmol/L,P=0.03)[63]。另外,将嗜酸乳杆菌、干酪乳杆菌、两歧双歧杆菌、发酵乳杆菌(各2×109 CFU/g每日)应用于对妊娠糖尿病孕妇的治疗,6周后,同样对FBG(β,-3.43 mg/dL;95% CI,-6.48,-0.38;P=0.02)、血浆胰岛素(β,-2.29 μIU/ mL;95% CI,-3.60,-0.99;P=-0.001)与HOMA-IR(β,-0.67;95% CI,-1.05,-0.29;P=0.001)有改善效果[64]。如前所述,益生菌的代谢产物SCFA有多种抗糖尿病活性。益生菌改善糖尿病的其他机制包括:(a)增强肠道紧密连接蛋白表达和屏障功能来减少肠道炎症[65];(b)恢复受损的肠道菌群多样性,减少有害菌的丰度,从而增强葡萄糖耐受[66];(c)通过清除自由基、螯合金属离子、自身产生抗氧化酶、调节肠道抗氧化酶表达发挥抗氧化作用[67];(d)抑制肠道中α-葡萄糖苷酶的活性,减少葡萄糖吸收[68]。
4.3 黄酮类
黄酮类化合物是植物的次生代谢产物,包括黄酮醇、黄酮、黄烷酮、异黄酮、黄烷醇和花青素等亚类,对糖尿病代谢紊乱有多种积极的影响。GDM大鼠接受桑叶总黄酮的治疗,糖脂代谢、炎症和氧化应激状态均得到显著改善[69]。将麦芪降糖丸与甘草黄酮联合治疗GDM,显著改善了患者FBG[(4.47±0.30)vs.(5.50±1.07) mmol/L,P=0.000]与2hPG[(5.70±1.34)vs.(7.50±1.07) mmol/L,P=0.000],减少不良妊娠结局的发生率(6.98%vs.23.81%,P=0.031)[70]。葛根素,一种异黄酮类化合物,能够降低妊娠糖尿病大鼠空腹血糖与氧化应激水平[71]。目前从植物中分离得到的黄酮类化合物有数千种,其改善糖尿病的机制不尽相同,如槲皮素改善GLUT4转位、抑制酪氨酸激酶活性并减少脂质过氧化;黄芩素抑制NF-κB途径和脂肪酸合成、激活肝脏中己糖激酶的活性与防止细胞凋亡;芦丁和花青素可通过抑制小肠中α-葡萄糖苷酶和α-淀粉酶的活性,从而减少碳水化合物的吸收[72]。
4.4 皂苷类
皂苷是苷元为三萜或螺甾烷类的糖苷类化合物,是许多中草药的有效活性成分。服用人参皂苷可显著改善GDM大鼠的IR,减少氧化应激与炎症反应,并改善妊娠结局[73]。罗汉果皂苷可缓解GDM大鼠的氧化应激损伤,从而保护胰腺组织[74]。皂苷可增强脂肪组织中PPARγ和脂联素的表达,增强GLUT4转位,改善胰岛素敏感性[75]。皂苷结构含有许多羟基,可与使葡萄糖氧化的金属离子螯合,而防止活性氧的产生[76]。皂苷通过刺激辣椒素敏感的感觉神经或增强回肠5-HT释放,抑制下丘脑的食欲信号,减少食物摄入[77]。
目前,经研究发现的膳食营养对GDM的主要改善机制如表1所示。
表1 膳食营养对GDM的主要改善机制
Table 1 The main improvement mechanism of dietary nutrition on GDM
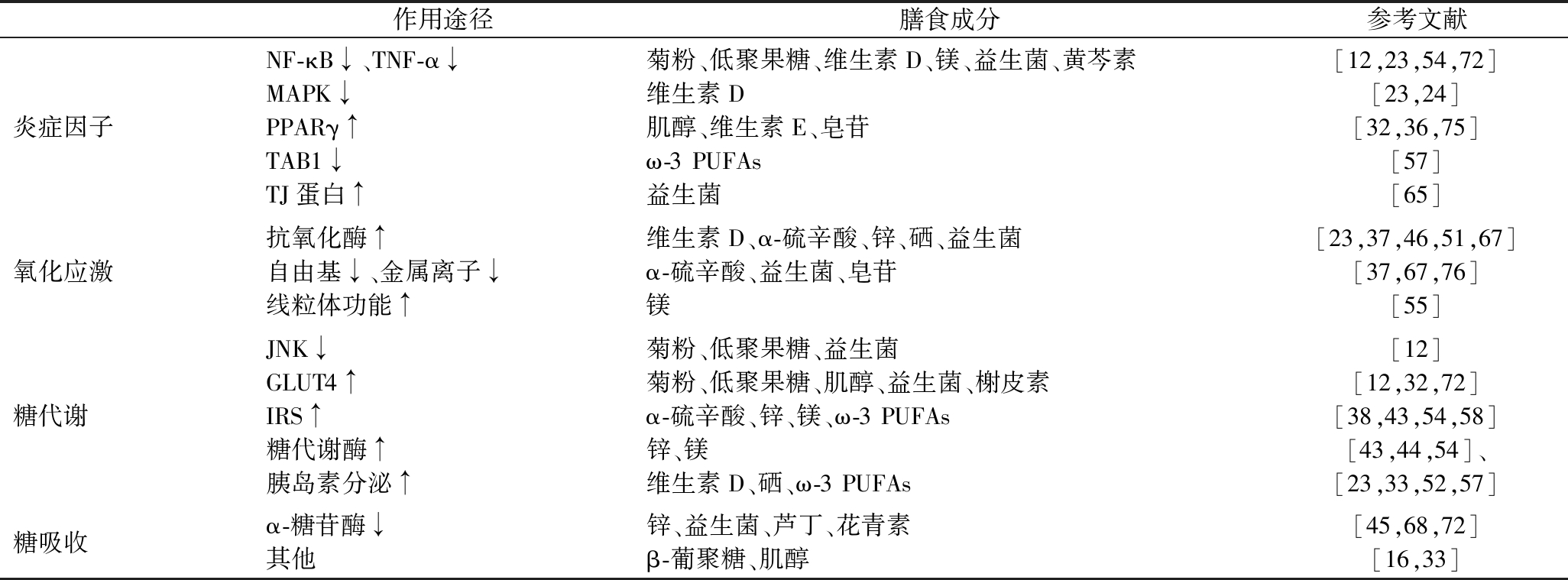
作用途径膳食成分参考文献炎症因子NF-κB↓、TNF-α↓MAPK↓PPARγ↑TAB1↓TJ蛋白↑菊粉、低聚果糖、维生素D、镁、益生菌、黄芩素维生素D肌醇、维生素E、皂苷ω-3PUFAs益生菌[12,23,54,72][23,24][32,36,75][57][65]氧化应激抗氧化酶↑自由基↓、金属离子↓线粒体功能↑维生素D、α-硫辛酸、锌、硒、益生菌α-硫辛酸、益生菌、皂苷镁[23,37,46,51,67][37,67,76][55]糖代谢JNK↓GLUT4↑IRS↑糖代谢酶↑胰岛素分泌↑菊粉、低聚果糖、益生菌菊粉、低聚果糖、肌醇、益生菌、榭皮素α-硫辛酸、锌、镁、ω-3PUFAs锌、镁维生素D、硒、ω-3PUFAs[12][12,32,72][38,43,54,58][43,44,54]、[23,33,52,57]糖吸收α-糖苷酶↓其他锌、益生菌、芦丁、花青素β-葡聚糖、肌醇[45,68,72][16,33]
5 膳食成分的协同作用
了解膳食成分间的协同增效关系对开发膳食干预策略有重要的指导意义。ω-3 PUFAs易发生氧化,而维生素的抗氧化特性能够缓解ω-3 PUFAs的氧化,从而增强ω-3 PUFAs的作用。另外,补充ω-3 PUFAs可能使体内的维生素D水平升高[78]。因此,ω-3 PUFAs与维生素可能发挥很好的协同作用。妊娠糖尿病孕妇每日摄入400 mg α-亚麻酸和400 IU维生素E,6周后显著降低FBG[(-11.8±11.0)vs.(+1.5±11.9) mg/dL,P<0.001)、血浆胰岛素[(-1.8±6.9)vs.(5.8±12.1) μIU/mL,P=0.004)与HOMA-IR(-0.8±1.6 vs.1.4±2.8,P=0.001)[79]。而每日2次服用40 000 IU维生素D和8 000 mg ω-3 PUFAs,6周后FBG[(-0.5±0.2)vs.(0.8±0.1) mmol/L,P<0.001]、血浆胰岛素[(-1.9±1.1)vs.(2.3±1.2) μIU/mL,P<0.001)与HOMA-IR(-0.4±0.2 vs.0.9±0.5,P<0.001)显著改善[80]。与单独服用维生素D或ω-3 PUFAs相比,联合补充对糖脂代谢、胰岛素敏感性与妊娠结局的影响更加显著[78,81]。
此外,益生菌能够增加肠道中维生素D受体基因的表达,维生素D能通过调节宿主免疫反应来调控肠道微生物群[82]。与仅益生菌干预相比,联合干预显著改善TG(b,-15.82,95% CI,-29.66,-1.98,P=0.02)与TAC(b,63.26,95% CI,18.25,108.26,P=0.006)等血脂与氧化应激状态[82]。与仅维生素D干预相比,联合干预显著降低FBG[(5.32±0.34)vs.(5.88±0.47) mmol/L,P<0.05]、2hPG[(6.51±1.12) vs.(7.61±1.24) mmol/L,P<0.05)与HOMA-IR(2.31±0.14 vs.2.89±0.24,P<0.05)[83]。
另外,益生元可选择性地刺激特定肠道菌的生长,改善肠道微生态,因此与益生菌可发挥协同作用。妊娠糖尿病孕妇每日服用一粒含有嗜酸乳杆菌、干酪乳杆菌与两歧双歧杆菌(各2×109 CFU/g),外加800 mg菊粉的胶囊,6周后显著改善血清胰岛素[(-1.5±5.9)vs.(+4.8±11.5) μIU/mL,P=0.005]、HOMA-IR(-0.4±1.3 vs.+1.1±2.7,P=0.003)与TAG(-14.8±56.5 vs.+30.4±37.8,P<0.001)[84]。
6 结论与展望
由于饮食等生活方式的变化,妊娠糖尿病的患病率逐年升高,如果没有得到及时的治疗,母亲与婴儿的身体健康将会受到极大的损害,而孕期对妊娠糖尿病的控制能够减少不良影响。医学营养支持是治疗妊娠糖尿病的主要措施,且良好的膳食控制效果能够减少后续药物的使用。因此,进行膳食干预的研究有重大的意义。本文总结了调控妊娠糖尿病的膳食纤维、维生素、矿物质等膳食功能性成分的应用进展及调控机制。
值得注意的是,目前许多食品组分对于妊娠糖尿病的改善作用还缺乏大量可靠的临床研究,大部分膳食成分的作用机制还停留在对二型糖尿病的研究上。未来的研究需要更加深入探索食品组分调控妊娠糖尿病的机理,进行更大样本量的有效性及安全性临床实验,挖掘更多新型的食品功能因子,以食品组分间的协同作用来指导实施联合干预措施。另外,妊娠糖尿病患者数量众多,且发病率逐年攀升,食品市场需求庞大,现有的特殊食品以全营养配方为主,非全营养食品较少见报道,相比于全营养食品,在膳食营养指导的基础上加以辅食干预应该有更高的接受度,因此基于膳食成分的改善作用以及它们的协同关系开发针对妊娠糖尿病的辅食型配方产品会有相当大的应用前景。
[1] GAO C H,SUN X,LU L,et al.Prevalence of gestational diabetes mellitus in mainland China:A systematic review and meta-analysis[J].Journal of Diabetes Investigation,2019,10(1):154-162.
[2] 李明.PI3K/AKT信号通路与妊娠期糖尿病胰岛素抵抗的关系[D].天津:天津医科大学,2010.
LI M.Relationship between PI3K/AKT signal pathway and insulin resistance in gestational diabetes mellitus[D].Tianjin:Tianjin Medical University,2010.
[3] 邬春莹.黄连素通过p38MAPK调节骨骼肌葡萄糖代谢的机制研究[D].广州:广州中医药大学,2018.
WU C Y.The mechanism of berberine in regulating skeletal muscle glucose metabolism via p38MAPK[D].Guangzhou:Guangzhou University of Chinese Medicine,2018.
[4] 李从青.GDM孕妇外周血单个核细胞在LPS刺激下TLR4的表达及其介导的NF-κB信号通路在GDM发病中的研究[D].合肥:安徽医科大学,2012.
LI C Q.Study on the expression of TLR4 in peripheral blood mononuclear cells of GDM pregnant women stimulated by LPS and its mediated NF-κB signaling pathway in the pathogenesis of GDM[D].Hefei:Anhui Medical University,2012.
[5] PONZO V,FEDELE D,GOITRE I,et al.Diet-gut microbiota interactions and gestational diabetes mellitus (GDM)[J].Nutrients,2019,11(2):1-3.
[6] 张恒,饶坤林.过氧化物酶增殖体激活受体γ与妊娠期糖尿病炎症反应的关系[J].中国临床医生杂志,2020,48(1):107-109.
ZHANG H,RAO K L.Relationship between peroxisome proliferator-activated receptor γ and inflammatory response in gestational diabetes mellitus[J].Chinese Journal for Clinicians,2020,48(1):107-109.
[7] 李佳.JNK信号转导通路在妊娠期糖尿病中作用的研究[D].西安:第四军医大学,2010.
LI J.Study on the role of JNK signal transduction pathway in gestational diabetes mellitus[D].Xi’an:The Fourth Military Medical University,2010.
[8] 苗苗,张悦,穆娟,等.菊粉型果聚糖对妊娠期糖尿病孕妇糖脂代谢的影响[J].江苏预防医学,2021,32(2):153-156.
MIAO M,ZHANG Y,MU J,et al.The effects of inulin-type fructans in pregnant women with gestational diabetes mellitus[J].Jiangsu Journal of Preventive Medicine,2021,32(2):153-156.
[9] NING C,WANG X Y,GAO S,et al.Chicory inulin ameliorates type 2 diabetes mellitus and suppresses JNK and MAPK pathways in vivo and in vitro[J].Molecular Nutrition &Food Research,2017,61(8):1-5.
[10] MIAO M,DAI Y M,RUI C,et al.Dietary supplementation of inulin alleviates metabolism disorders in gestational diabetes mellitus mice via RENT/AKT/IRS/GLUT4 pathway[J].Diabetology &Metabolic Syndrome,2021,13(1):150.
[11] LI K,ZHANG L,XUE J,et al.Dietary inulin alleviates diverse stages of type 2 diabetes mellitus via anti-inflammation and modulating gut microbiota in db/db mice[J].Food &Function,2019,10(4):1915-1927.
[12] 邓邦利.钙信号和短链脂肪酸调节糖代谢机制研究[D].天津:天津医科大学,2018.
DENG B L.Study on the mechanism of calcium signaling and short-chain fatty acids regulating glucose metabolism[D].Tianjin:Tianjin Medical University,2018.
[13] 刘争艳.低聚果糖联合个体化营养治疗对妊娠期糖尿病患者临床疗效的影响[J].数理医药学杂志,2021,34(6):941-942.
LIU Z Y.Effect of oligofructose combined with individualized nutrition on the clinical efficacy of gestational diabetes mellitus[J].Journal of Mathematical Medicine,2021,34(6):941-942.
[14] 王蕾蕾.燕麦对妊娠期糖尿病孕妇肠道菌群的影响[D].上海:上海交通大学,2019.
WANG L L.Effects of oatmeal on intestinal flora of pregnant women with gestational diabetes mellitus[D].Shanghai:Shanghai Jiao Tong University,2019.
[15] BARATI Z,IRAVANI M,KARANDISH M,et al.The effect of oat bran consumption on gestational diabetes:A randomized controlled clinical trial[J].BMC Endocrine Disorders,2021,21(1):67.
[16] ZHANG J,LUO K Y,ZHANG G Y.Impact of native form oat β-glucan on starch digestion and postprandial glycemia[J].Journal of Cereal Science,2017,73:84-90.
[17] 张洁.燕麦颗粒中谷粒态β-葡聚糖对淀粉消化以及糖脂代谢的影响[D].无锡:江南大学,2016.
ZHANG J.Effects of grain-state β-glucan in oat granules on starch digestion and glycolipid metabolism[D].Wuxi:Jiangnan University,2016.
[18] 吕荣梅.小麦纤维素颗粒添加疗法对GDM糖脂代谢及妊娠结局的影响[J].实用糖尿病杂志,2020,16(4):20.
LYU R M.Effect of wheat cellulose granule addition therapy on glucose and lipid metabolism and pregnancy outcome of GDM[J].Journal of Practical Diabetology,2020,16(4):20.
[19] 孙晓峰,麦子霞,丘文君,等.小麦纤维素在妊娠期糖尿病(GDM)治疗中的应用[J].吉林医学,2016,37(2):274-276.
SUN X F,MAI Z X,QIU W J,et al.The study of testa triticum tricum purify in the treatment of gestational diabetes mellitus[J].Jilin Medical Journal,2016,37(2):274-276.
[20] AFAGHI A,GHANEI L,ZIAEE A.Effect of low glycemic load diet with and without wheat bran on glucose control in gestational diabetes mellitus:A randomized trial[J].Indian Journal of Endocrinology and Metabolism,2013,17(4):689-692.
[21] YAZDCHI R,GARGARI B P,ASGHARI-JAFARABADI M,et al.Effects of vitamin D supplementation on metabolic indices and hs-CRP levels in gestational diabetes mellitus patients:A randomized,double-blinded,placebo-controlled clinical trial[J].Nutrition Research and Practice,2016,10(3):328-335.
[22] ASEMI Z,KARAMALI M,ESMAILLZADEH A.Favorable effects of vitamin D supplementation on pregnancy outcomes in gestational diabetes:A double blind randomized controlled clinical trial[J].Hormones et Metabolisme,2015,47(8):565-570.
[23] SZYMCZAK-PAJOR I,DRZEWOSKI J, LIWI
LIWI SKA A.The molecular mechanisms by which vitamin D prevents insulin resistance and associated disorders[J].International Journal of Molecular Sciences,2020,21(18):6644.
SKA A.The molecular mechanisms by which vitamin D prevents insulin resistance and associated disorders[J].International Journal of Molecular Sciences,2020,21(18):6644.
[24] NIMITPHONG H,PARK E,LEE M J.Vitamin D regulation of adipogenesis and adipose tissue functions[J].Nutrition Research and Practice,2020,14(6):553-567.
[25] 刘军,赵康,马艳,等.维生素D联合有氧运动通过调控肝脏PI3K/Akt信号通路改善db/db小鼠胰岛素抵抗[J].西安体育学院学报,2020,37(6):742-749.
LIU J,ZHAO K,MA Y,et al.Vitamin D combined with aerobic exercise improves insulin resistance in db/db mice by regulating PI3K/Akt signaling pathway in liver[J].Journal of Xi’an Physical Education University,2020,37(6):742-749.
[26] 吴群.维生素B12联合叶酸对妊娠期糖尿病患者血糖及妊娠结局的影响[J].中国乡村医药,2020,27(10):5-6.
WU Q.Effect of vitamin B12 combined with folic acid on blood sugar and pregnancy outcome in patients with gestational diabetes mellitus[J].Chinese Journal of Rural Medicine and Pharmacy,2020,27(10):5-6.
[27] 田艳柳,杨霞.叶酸、维生素B6、甲钴铵联合门冬胰岛素治疗GDM合并HHcy患者的效果及对围产儿并发症的影响[J].临床医学研究与实践,2018,3(30):148-149.
TIAN Y L,YANG X.Effect of folic acid,vitamin B6,methylcobalamin combined with insulin aspart in the treatment of GDM combined with HHcy patients and its effect on perinatal complications[J].Clinical Research and Practice,2018,3(30):148-149.
[28] KULSHRESTHA V,BALANI S,KACHHAWA G,et al.Efficacy of myoinositol in treatment of gestational diabetes mellitus in Asian Indian women:A pilot randomized clinical trial[J].European Journal of Obstetrics &Gynecology and Reproductive Biology,2021,260:42-47.
[29] CORRADO F,D’ANNA R,VIESTE G D,et al.The effect of myoinositol supplementation on insulin resistance in patients with gestational diabetes[J].Diabetic Medicine:a Journal of the British Diabetic Association,2011,28(8):972-975.
[30] MASCOLO E,VERN F.Vitamin B6 and diabetes:Relationship and molecular mechanisms[J].International Journal of Molecular Sciences,2020,21(10):3669.
F.Vitamin B6 and diabetes:Relationship and molecular mechanisms[J].International Journal of Molecular Sciences,2020,21(10):3669.
[31] YADAV D K,SHRESTHA S,LILLYCROP K A,et al.Vitamin B12 supplementation influences methylation of genes associated with type 2 diabetes and its intermediate traits[J].Epigenomics,2018,10(1):71-90.
[32] ANTONY P J,GANDHI G R,STALIN A,et al.Myoinositol ameliorates high-fat diet and streptozotocin-induced diabetes in rats through promoting insulin receptor signaling[J].Biomedicine &Pharmacotherapy,2017,88:1098-1113.
[33] CHUKWUMA C I,IBRAHIM M A,ISLAM M S.Myo-inositol inhibits intestinal glucose absorption and promotes muscle glucose uptake:A dual approach study[J].Journal of Physiology and Biochemistry,2016,72(4):791-801.
[34] 陈丽华,张小红.维生素E对妊娠糖尿病患者血脂及妊娠结局的影响[J].中国妇幼健康研究,2018,29(7):933-935.
CHEN L H,ZHANG X H.Effect of vitamin E on blood lipids and pregnancy outcomes in patients with gestational diabetes mellitus[J].Chinese Journal of Woman and Child Health Research,2018,29(7):933-935.
[35] 黄健容,黄琳琳.维生素E对妊娠糖尿病患者CRP、IL-6、IL-8及脂类水平的影响[J].海南医学院学报,2015,21(12):1658-1660.
HUANG J R,HUANG L L.Effects of vitamin E on CRP,IL-6,IL-8 and lipid levels in patients with gestational diabetes mellitus[J].Journal of Hainan Medical University,2015,21(12):1658-1660.
[36] GRAY B,SWICK J,RONNENBERG A G.Vitamin E and adiponectin:Proposed mechanism for vitamin E-induced improvement in insulin sensitivity[J].Nutrition Reviews,2011,69(3):155-161.
[37] 黄自强,庞云渭,郝海生,等.α-硫辛酸抗氧化作用机制及其在动物生殖细胞和早期胚胎中抗氧化作用的研究进展[J].中国畜牧杂志,2019,55(3):6-12.
HUANG Z Q,PANG Y W,HAO H S,et al.Antioxidant mechanisms of alpha lipoic acid and its research progress on animal germ cells and early embryos[J].Chinese Journal of Animal Science,2019,55(3):6-12.
[38] QIN Z Y,ZHANG M,GUO X R,et al.α-Lipoic acid ameliorates impaired glucose uptake in LYRM1 overexpressing 3T3-L1 adipocytes through the IRS-1/Akt signaling pathway[J].Journal of Bioenergetics and Biomembranes,2012,44(5):579-586.
[39] TARGONSKY E D,DAI F,KOSHKIN V,et al.α-Lipoic acid regulates AMP-activated protein kinase and inhibits insulin secretion from beta cells[J].Diabetologia,2006,49(7):1587-1598.
[40] ASLFALAH H,JAMILIAN M,RAFIEI F,et al.Reduction in maternal serum values of glucose and gamma-glutamyltransferase after supplementation with alpha-lipoic acid in women with gestational diabetes mellitus[J].The Journal of Obstetrics and Gynaecology Research,2019,45(2):313-317.
[41] KARAMALI M,HEIDARZADEH Z,SEIFATI S M,et al.Zinc supplementation and the effects on metabolic status in gestational diabetes:A randomized,double-blind,placebo-controlled trial[J].Journal of Diabetes and Its Complications,2015,29(8):1314-1319.
[42] MIRANDA E R,DEY C S.Effect of chromium and zinc on insulin signaling in skeletal muscle cells[J].Biological Trace Element Research,2004,101(1):19-36.
[43] ILOUZ R,KAIDANOVICH O,GURWITZ D,et al.Inhibition of glycogen synthase kinase-3β by bivalent zinc ions:Insight into the insulin-mimetic action of zinc[J].Biochemical and Biophysical Research Communications,2002,295(1):102-106.
[44] CANESI L,BETTI M,CIACCI C,et al.Insulin-like effect of zinc in Mytilus digestive gland cells:Modulation of tyrosine kinase-mediated cell signaling[J].General and Comparative Endocrinology,2001,122(1):60-66.
[45] ZENG Y F,LEE J,SI Y X,et al.Inhibitory effect of Zn2+ on α-glucosidase:Inhibition kinetics and molecular dynamics simulation[J].Process Biochemistry,2012,47(12):2510-2517.
[46] LIMA V B,SAMPAIO F D E A,BEZERRA D L,et al.Parameters of glycemic control and their relationship with zinc concentrations in blood and with superoxide dismutase enzyme activity in type 2 diabetes patients[J].Arquivos Brasileiros De Endocrinologiae Metabologia,2011,55(9):701-707.
[47] ASEMI Z,JAMILIAN M,MESDAGHINIA E,et al.Effects of selenium supplementation on glucose homeostasis,inflammation,and oxidative stress in gestational diabetes:Randomized,double-blind,placebo-controlled trial[J].Nutrition,2015,31(10):1235-1242.
[48] JAMILIAN M,SAMIMI M,EBRAHIMI F A,et al.Effects of selenium supplementation on gene expression levels of inflammatory cytokines and vascular endothelial growth factor in patients with gestational diabetes[J].Biological Trace Element Research,2018,181(2):199-206.
[49] KARAMALI M,DASTYAR F,BADAKHSH M H,et al.The effects of selenium supplementation on gene expression related to insulin and lipid metabolism,and pregnancy outcomes in patients with gestational diabetes mellitus:A randomized,double-blind,placebo-controlled trial[J].Biological Trace Element Research,2020,195(1):1-8.
[50] SADAT NAJIB F,POORDAST T,REZVAN NIA M,et al.Effects of selenium supplementation on glucose homeostasis in women with gestational diabetes mellitus:A randomized,controlled trial[J].International Journal of Reproductive BioMedicine (IJRM),2020,18(1):57-64.
[51] KONG F J,MA L L,CHEN S P,et al.Serum selenium level and gestational diabetes mellitus:A systematic review and meta-analysis[J].Nutrition Journal,2016,15(1):1-10.
[52] CAMPBELL S C,ALDIBBIAT A,MARRIOTT C E,et al.Selenium stimulates pancreatic beta-cell gene expression and enhances islet function[J].FEBS Letters,2008,582(15):2333-2337.
[53] JAMILIAN M,SAMIMI M,FARANEH A E,et al.Magnesium supplementation affects gene expression related to insulin and lipid in patients with gestational diabetes[J].Magnesium Research,2017,30(3):71-79.
[54] FENG J N,WANG H Y,JING Z,et al.Role of magnesium in type 2 diabetes mellitus[J].Biological Trace Element Research,2020,196(1):74-85.
[55] LIU M,JEONG E M,LIU H,et al.Magnesium supplementation improves diabetic mitochondrial and cardiac diastolic function[J].JCI Insight,2019,4(1):e123182.
[56] ELSHANI B,KOTORI V,DACI A.Role of omega-3 polyunsaturated fatty acids in gestational diabetes,maternal and fetal insights:Current use and future directions[J].The Journal of Maternal-Fetal &Neonatal Medicine,2021,34(1):124-136.
[57] OH D Y,WALENTA E.Omega-3 fatty acids and FFAR4[J].Frontiers in Endocrinology,2014,5:115.
[58] KWON Y.Immuno-resolving ability of resolvins,protectins,and maresins derived from omega-3 fatty acids in metabolic syndrome[J].Molecular Nutrition &Food Research,2020,64(4):e1900824.
[59] FATIMA QAZI A,MUHAMMAD SHAIKH D.Ameliorating effects of omega-3 fatty acids on underlying mechanisms of type 2 diabetes[J].Journal of Pharmaceutical Research International,2019,31(6):1-7.
[60] OZYAZGAN S,KARAOGLU K,KURT A,et al.Effects of omega-3 polyunsaturated fatty acid supplementation on serum fetuin-A levels in type 2 diabetic patients[J].Minerva Medica,2013,104(3):287-293.
[61] SAMIMI M,JAMILIAN M,ASEMI Z,et al.Effects of omega-3 fatty acid supplementation on insulin metabolism and lipid profiles in gestational diabetes:Randomized,double-blind,placebo-controlled trial[J].Clinical Nutrition,2015,34(3):388-393.
[62] JAMILIAN M,TABASSI Z,REINER Ž,et al.The effects of n-3 fatty acids from flaxseed oil on genetic and metabolic profiles in patients with gestational diabetes mellitus:A randomised,double-blind,placebo-controlled trial[J].British Journal of Nutrition,2020,123(7):792-799.
[63] BADEHNOOSH B,KARAMALI M,ZARRATI M,et al.The effects of probiotic supplementation on biomarkers of inflammation,oxidative stress and pregnancy outcomes in gestational diabetes[J].The Journal of Maternal-Fetal &Neonatal Medicine,2018,31(9):1128-1136.
[64] BABADI M,KHORSHIDI A,AGHADAVOOD E,et al.The effects of probiotic supplementation on genetic and metabolic profiles in patients with gestational diabetes mellitus:A randomized,double-blind,placebo-controlled trial[J].Probiotics and Antimicrobial Proteins,2019,11(4):1227-1235.
[65] PATEL R M,MYERS L S,KURUNDKAR A R,et al.Probiotic bacteria induce maturation of intestinal claudin 3 expression and barrier function[J].The American Journal of Pathology,2012,180(2):626-635.
[66] ZHENG Q X,JIANG X M,WANG H W,et al.Probiotic supplements alleviate gestational diabetes mellitus by restoring the diversity of gut microbiota:A study based on 16S rRNA sequencing[J].Journal of Microbiology,2021,59(9):827-839.
[67] FENG T,WANG J.Oxidative stress tolerance and antioxidant capacity of lactic acid bacteria as probiotic:A systematic review[J].Gut Microbes,2020,12(1):1801944.
[68] CHEN P,ZHANG Q X,DANG H,et al.Screening for potential new probiotic based on probiotic properties and α-glucosidase inhibitory activity[J].Food Control,2014,35(1):65-72.
[69] 史纪芳,潘佳琪,陈梦,等.基于PPARγ途径探讨桑叶总黄酮对妊娠期糖尿病模型大鼠糖脂代谢、炎症和氧化应激的改善作用[J].中国药房,2020,31(6):671-676.
SHI J F,PAN J Q,CHEN M,et al.Improvement effects of total flavonoids from Morus alba on glycolipid metabolism,inflammation and oxidative stress in gestational diabetes mellitus model rats based on PPARγ pathway[J].China Pharmacy,2020,31(6):671-676.
[70] 马秀玲.麦芪降糖丸联合甘草黄酮对妊娠期糖尿病患者血糖控制及妊娠结局的影响[J].现代医用影像学,2018,27(4):1373-1374.
MA X L.Effect of Maiqi Jiangtang Pill combined with Glycyrrhiza flavonoids on blood sugar control and pregnancy outcome in patients with gestational diabetes mellitus[J].Modern Medical Imagelogy,2018,27(4):1373-1374.
[71] 聂晓霞,王翠香.葛根素提取物改善妊娠期糖尿病大鼠的氧化应激损伤[J].现代食品科技,2021,37(2):44-48;63.
NIE X X,WANG C X.Puerarin improves oxidative stress in rats with gestational diabetes mellitus[J].Modern Food Science and Technology,2021,37(2):44-48;63.
[72] AL-ISHAQ R K,ABOTALEB M,KUBATKA P,et al.Flavonoids and their anti-diabetic effects:Cellular mechanisms and effects to improve blood sugar levels[J].Biomolecules,2019,9(9):430.
[73] 丁敬,冷在华,张秀琼.人参皂苷Re通过内质网应激通路对妊娠期糖尿病大鼠妊娠结局的影响及相关机制[J].临床和实验医学杂志,2021,20(8):804-808.
DING J,LENG Z H,ZHANG X Q.Effect of ginsenoside Re on the pregnancy outcome of gestational diabetic rats through the endoplasmic reticulum stress pathway and related mechanisms[J].Journal of Clinical and Experimental Medicine,2021,20(8):804-808.
[74] 于万芹,杜晓娜,刘巧敏,等.罗汉果皂苷对妊娠糖尿病大鼠氧化应激损伤影响[J].中国临床药理学杂志,2019,35(21):2723-2727.
YU W Q,DU X N,LIU Q M,et al.Effects of Momordica grosvenori saponin on oxidative stress injury in gestational diabetic rats[J].The Chinese Journal of Clinical Pharmacology,2019,35(21):2723-2727.
[75] KWON D Y,KIM Y S,RYU S Y,et al.Platyconic acid,a saponin from Platycodi radix,improves glucose homeostasis by enhancing insulin sensitivity in vitro and in vivo[J].European Journal of Nutrition,2012,51(5):529-540.
[76] ELEKOFEHINTI O O.Saponins:Anti-diabetic principles from medicinal plants:A review[J].Pathophysiology,2015,22(2):95-103.
[77] HAMAO M,MATSUDA H,NAKAMURA S,et al.Anti-obesity effects of the methanolic extract and chakasaponins from the flower buds of Camellia sinensis in mice[J].Bioorganic &Medicinal Chemistry,2011,19(20):6033-6041.
[78] JAMILIAN M,SAMIMI M,EBRAHIMI F A,et al.The effects of vitamin D and omega-3 fatty acid co-supplementation on glycemic control and lipid concentrations in patients with gestational diabetes[J].Journal of Clinical Lipidology,2017,11(2):459-468.
[79] TAGHIZADEH M,JAMILIAN M,MAZLOOMI M,et al.A randomized-controlled clinical trial investigating the effect of omega-3 fatty acids and vitamin E co-supplementation on markers of insulin metabolism and lipid profiles in gestational diabetes[J].Journal of Clinical Lipidology,2016,10(2):386-393.
[80] HUANG S Z,FU J F,ZHAO R X,et al.The effect of combined supplementation with vitamin D and omega-3 fatty acids on blood glucose and blood lipid levels in patients with gestational diabetes[J].Annals of Palliative Medicine,2021,10(5):5652-5658.
[81] RAZAVI M,JAMILIAN M,SAMIMI M,et al.The effects of vitamin D and omega-3 fatty acids co-supplementation on biomarkers of inflammation,oxidative stress and pregnancy outcomes in patients with gestational diabetes[J].Nutrition &Metabolism,2017,14(1):1-9.
[82] JAMILIAN M,AMIRANI E,ASEMI Z.The effects of vitamin D and probiotic co-supplementation on glucose homeostasis,inflammation,oxidative stress and pregnancy outcomes in gestational diabetes:A randomized,double-blind,placebo-controlled trial[J].Clinical Nutrition,2019,38(5):2098-2105.
[83] 杨艳,叶佳,杨敏,等.益生菌结合维生素D对妊娠期糖尿病糖脂代谢、胰岛素抵抗的影响[J].解放军医药杂志,2020,32(11):71-74.
YANG Y,YE J,YANG M,et al.Effects of probiotics combined with vitamin D on glucose-lipid metabolism and insulin resistance in patients with gestational diabetes mellitus[J].Medical &Pharmaceutical Journal of Chinese PLA,2020,32(11):71-74.
[84] AHMADI S,JAMILIAN M,TAJABADI-EBRAHIMI M,et al.The effects of synbiotic supplementation on markers of insulin metabolism and lipid profiles in gestational diabetes:A randomised,double-blind,placebo-controlled trial[J].The British Journal of Nutrition,2016,116(8):1394-1401.